Apart from the humanitarian crisis, the aftermath of the second wave of the pandemic has created a huge pile-up of biomedical waste. Experts and doctors say it is a ticking time bomb as far as waste management is concerned. The pile-up of large amounts of biomedical waste has presented an unprecedented challenge to civic bodies in most of the majority of cities in the world with regards to their disposal.
More than 300 kg of waste is being generated every day, which includes disposable tableware, plastic, packaging material etc., that is used by patients at homes, covid centres and hospitals.
A Brief About Biomedical Waste Disposal and Collection
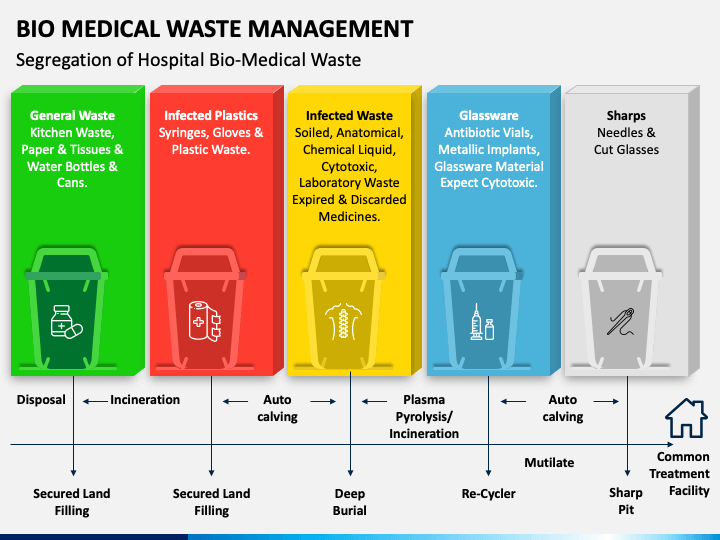
Image Source: https://www.sketchbubble.com/en/presentation-bio-medical-waste-management.html
We know that biomedical waste is collected in four colour-coded bags namely–
- Yellow (Cotton wastes, pathological wastes, dressing materials, face mask, cap, cytotoxic products, expired, discarded medicines, microbiological and biotechnology lab wastes)
- Red (syringes with needles,iv sets,catheters,gloves,urine bag,dialysis kit,IV bottles,plastic wastes,goggles)
- White (Needles, syringes with fixed needles, blades, scalpels)
- Blue (broken glass, Ampoules, lab slides, metallic body implants, nails, scissors)
COVID-19 patients and their caretakers are advised to separate wet and dry waste and spray it with sodium hypochlorite before disposing it in the yellow garbage bag and handing them over to the waste collector. The administration in most cities has made special arrangements for the collection of tissues and face masks from quarantined homes such that they are not mixed with general waste.
Some Eye-Popping Statics About Biomedical Waste
The total amount of waste generated by healthcare activities is about 85%, which is considered general, non-hazardous waste. The remaining 15% is considered hazardous as it is either infectious, toxic or radioactive.
Around 16 billion injections are administered worldwide. Open burning and incineration of health care wastes can come under some circumstances result in the emission of dioxins, furans, and hazardous particulate matter.

Image Source: https://swachhindia.ndtv.com/coronavirus-pandemic-exposes-broken-system-of-bio-medical-waste-management-experts-discuss-the-issue-and-solutions-49427/
Coming closer home, the ongoing covid-19 pandemic revealed not just India’s poor healthcare system but also the many voids in its waste management system. Did you know that India generates around 101 Metric Tonnes (MT) of COVID-19 -related waste every day? Well, this number is over and above the usual biomedical waste quantity of 609 MT that the country produces each day. What is alarming is that the available capacity for incinerating biomedical waste in the country is 840 MT and we already produce 710 MT per day! (As per a report filed by the Central Pollution Control Board (CPCB) in the National Green Tribunal in July 2020)
Measures to create safe and environmentally sound management of healthcare wastes can prevent adverse health and environmental impacts from such wastes raising the release of chemical or biological hazards, including drug-resistant microorganisms, into the environment which is protecting the health of patients and healthcare workers and the general public.
Types of Biomedical Waste

Image Source: Image by Viktor Ivanchenko from Pixabay
Infectious waste: Waste that is contaminated with blood and other bodily fluids e.g.discarded diagnostic samples, cultures and stocks of infectious agents from laboratory work (waste from autopsies and infected animals from laboratories), waste from patients with infections e.g. swabs, bandages and disposable medical devices.
Pathological waste: Wastes like human tissues, organs or fluids, body parts and contaminated animal carcasses.
Sharps: Syringes, needles, disposable scalpels and blades, etc.
Chemical waste: Solvents and reagents used for laboratory preparations, disinfectants, sterilants and heavy metals contained in medical devices like mercury in broken thermometers and batteries.
Pharmaceutical waste: Expired, unused and contaminated drugs and vaccines.
Cytotoxic waste: Waste containing substances with genotoxic properties (i.e. highly hazardous substances that are, mutagenic, teratogenic or carcinogenic), such as cytotoxic drugs used in cancer treatment and their metabolites.
Radioactive waste: Wastes such as products contaminated by radionuclides including radioactive diagnostic material or radiotherapeutic materials.
General waste: Waste that does not pose any particular biological, chemical, radioactive or physical hazards
The major sources of healthcare waste are:
- Hospitals and other health facilities
- Laboratories and research centres
- Mortuary and autopsy centres
- Animal research and testing laboratories
- Blood banks and collection services
- Nursing homes for the elderly
According to statistics, it is believed that around 0.5 kg of hazardous waste per hospital bed per day is produced in high-income countries, while the same in low-income countries remains around an average of 0.2 kg.
What Are The Healthcare Risks of Biomedical Waste?
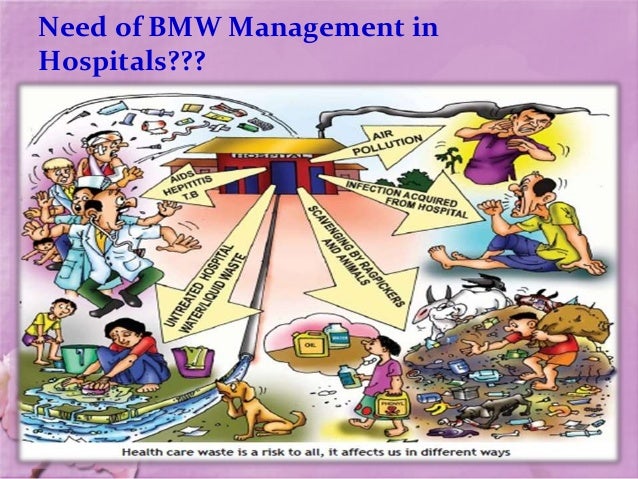
Image Source: https://www.slideshare.net/DAYANAJOSE002/biomedical-waste-management-50494443
Healthcare waste contains potentially harmful microorganisms that can infect hospital patients, health workers and the general public. Other potential hazards may include drug-resistant microorganisms which spread from health facilities into the environment.
Adverse health outcomes associated with health care waste and by-products include:
- Sharps-inflicted injuries
- Toxic exposure to pharmaceutical products, especially antibiotics and cytotoxic drugs released into the surrounding environment, and to substances such as mercury or dioxins, during the handling or incineration of health care wastes
- Chemical burns arising in the context of disinfection, sterilization or waste treatment activities
- Air pollution arising as a result of the release of particulate matter during medical waste incineration
- Thermal injuries occurring in conjunction with open burning and the operation of medical waste incinerators.
- Radiation burns.
- Sharps-related
Worldwide, an estimated 16 billion injections are administered every year. Not all needles and syringes are disposed of safely, creating a risk of injury and infection and opportunities for reuse.
Injections with contaminated needles and syringes in low and middle-income countries have reduced substantially in recent years, partly due to efforts to reduce the reuse of injection devices. Despite this progress, in 2010, unsafe injections were still responsible for as many new HIV infections, hepatitis B infections and hepatitis C infections.
A person who experiences one needle stick injury from a needle used on an infected source patient has risks of 30%, 1.8%, and 0.3% respectively of becoming infected with HBV, HCV and HIV respectively.
Additional hazards occur from scavenging at waste disposal sites and during the handling and manual sorting of hazardous waste from healthcare facilities. These practices are common in many regions of the world, especially in low and middle-income countries. The waste handlers are at immediate risk of needle-stick injuries and exposure to toxic or infectious materials.
Environmental Impact of Biomedical Waste

Image Source: https://www.arre.co.in/coronavirus/coronavirus-oceans-biomedical-waste-oceans/
The release of pathogens and toxic pollutants into the environment can pose a direct and indirect risk to health. The improper disposal of untreated health care wastes in landfills can lead to the contamination of drinking, surface, and groundwater if those landfills are not properly constructed.
The treatment of healthcare wastes with chemical disinfectants can result in the release of chemical substances into the environment if those substances are not handled, stored and disposed of in an environmentally sound manner.
Incineration of waste has been widely practised, but inadequate incineration of unsuitable materials results in the release of pollutants into the air and in the generation of ash residue. Incinerated materials containing or treated with chlorine can generate dioxins and furans, which are human carcinogens and have been associated with a range of adverse health effects.
Incineration of heavy metals or materials with high metal content (particular lead, mercury and cadmium) can lead to the spread of toxic metals in the environment. Only modern incinerators operating at 850 -1100 °C and fitted with special gas cleaning equipment can comply with the international emission standards for dioxins and furans.
Alternatives to incineration such as autoclaving, microwaving, steam treatment integrated with internal mixing can minimize the formation and release of chemicals or hazardous emissions should be considered in settings where there are sufficient resources to operate and maintain such systems and dispose of the treated waste.
How To Improve Healthcare Waste Management?
To promote practices that reduce the volume of wastes generated and ensure proposer waste segregation across the globe, countries need to develop strategies and systems along with strong oversight and regulation to incrementally improve waste segregation, destruction and disposal practices. These efforts need to be made with the ultimate aim of meeting national and international standards wherever feasible while favouring the safe and environmentally sound treatment of hazardous health care wastes.
This is a long-term process, sustained by gradual improvements; raising awareness of the risks related to healthcare waste, and of safe practices and selecting environmentally-friendly management options when collecting, handling, storing, transporting, treating or disposing of waste.
The commitment and support from various governments commitment are needed for universal, long-term improvement, although immediate action can be taken locally.
WHO developed the first global and comprehensive guidance document, Safe management of wastes from healthcare activities, now in its second edition and more recently a short guide that summarizes the key elements.
The guide addresses aspects such as regulatory framework, planning issues, waste minimization and recycling, handling, storage and transportation, treatment and disposal options, and training. The document is aimed at managers of hospitals and other healthcare facilities, policymakers, public health professionals and managers involved in waste management.
The WHO/UNICEF Joint Monitoring Programme will regularly report on the safe management of health care waste as part of wider monitoring efforts on water and sanitation in health care facilities.
In collaboration with other partners, WHO also developed a series of training modules on good practices in healthcare waste management covering all aspects of waste management activities from identification and classification of wastes to considerations guiding their safe disposal using both non-incineration or incineration strategies.
The Takeaway
The COVID-19 pandemic has laid open the bare insufficiency embedded in the waste management system existing in the world today. In the current scenario, it is indeed a wake-up call that must lead to stricter monitoring of biomedical waste management at every level in society.










Comments